Author: Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
The World Antimicrobial Awareness Week (WAAW) is celebrated annually from 18th to 24th November. It aims to increase awareness of global anti-microbial resistance (AMR) and to encourage best practices among the general public, healthcare workers and policy makers to avoid the further emergence and spread of drug-resistant infections. On occasion of WAAW, PARAS PATHOLOGY would like to contribute by educating about AMR.
What is an anti-microbial?
Anti-microbial are medicines used to prevent and treat infections caused by disease causing micro-organisms in humans, animals and plants. These include antibiotics, antivirals, antifungals and anti-parasitics. In common language, we usually use anti-biotics as a blanket term for these anti-microbials, but strictly speaking, antibiotics work against disease causing bacteria, antivirals against viruses, antifungals against fungus and antiparasitic against parasites. All these disease causing agents are collectively called pathogens.
Until the 19th century, it was difficult to treat infections, as there were no targeted anti-microbials for infections. In early 20th century, Alexander Fleming discovered the antibiotic penicillin, the first direct demonstration of an antibiotic in action, and it led to the development of an important field of science! Suddenly, infections started to seem treatable, and this was put to the ultimate test during the world wars to treat wound infections: it was proved beyond doubt that anti-biotics save lives!
What is Anti-Microbial Resistance (AMR)?
AMR occurs when bacteria, viruses, fungi and parasites no longer respond to medicines, thus making infections harder to treat and increasing the risk of disease spread, severe illness and death. In very simple words, AMR is said to develop when germs are not killed by the medicines designed to kill them and continue to grow in spite of taking these medicine. AMR does not mean the “human body” is becoming resistant to antimicrobials; AMR is related to the germs, not our body.
Why is AMR a global concern?
It is indeed unfortunate that within 100 years of discovery of penicillin, it was used so rampantly that it became ineffective against most common infections.
The emergence and spread of drug-resistant pathogens that have acquired new resistance mechanisms, leading to antimicrobial resistance, continue to threaten our ability to treat common infections. Especially alarming is the rapid global spread of multi-resistant and pan-resistant bacteria (also known as “superbugs”) that cause infections that are not treatable with existing antimicrobials or treated with higher doses and/or longer treatment duration. Thus, infections caused by such superbugs require extended hospital stays, additional follow-up doctor visits, high cost of treatment, physical disability, and in worst cases death.
The development of new anti-microbial, including research, development, human trials, etc. takes many years, even decades. However, indiscriminate use of anti-microbials has accelerated the development of AMR to the level of being faster than we can catch up! In this regard, it is the responsibility of both patient as well as treating doctors to prevent AMR, otherwise soon we will be running out of effective antibiotics. Thus, AMR is aptly being recognized as a growing pandemic, without any resolution in sight!
What accelerates the emergence and spread of AMR?
Anti-microbials if used in an appropriate dosage, for an appropriate length of time is unlikely to cause AMR. Therefore, in the simplest terms, the main drivers of AMR include the misuse and overuse of anti-microbials.
Patient’s role in prevention of AMR:
· Do not use anti-microbial drugs as “over the counter (OTC)” drugs. Antibiotics should always be taken under recommendation and supervision of a medical doctor.
· Whenever you are prescribed antibiotics by your family doctor, finish the full course even if you are feeling better after few doses.
· Don’t skip or miss any of your doses.
Treating Doctor’s role in prevention of AMR:
Whenever necessary, ask for a culture and sensitivity test to know the disease causing bacteria and its sensitivity pattern before starting antibiotics. A culture and sensitivity test is particularly important for patients with recurring infections, and infections in children. In case of clinical emergency one can start with empirical treatment and once report is received taper empirical therapy and shift to targeted treatment on basis of sensitivity pattern.
Practical challenges which promote AMR & its solutions:
1: Cost of treatment
Solution: Cost of antibiotic therapy may be higher than culture and sensitivity test, besides exposing the patient to side effects of taking multiple antibiotics. Blanket therapy with multiple antibiotics is costlier than treating with single antibiotic after a culture and sensitivity report.
2: Delay in reports. Even in best scenario culture and sensitivity report takes 24 to 48 hours.
Solution: Depending on clinical scenario one can take a call to wait till culture report or not. In case of emergency, ask the clinical microbiologist for gram stain report which can be provided in an hour of sample collection. One can take a call for starting empirical antibiotic course on basis of whether Gram positive or Gram negative organism seen on gram stain. Once report is received taper empirical treatment and switch to targeted therapy.
3: Urgency (non-medical) of the patient to get better!
Solution: AMR is related to the community at large. We all need to stand together, patients and doctors, and encourage each other to prevent misuse of anti-microbials. There is no “MAGIC DRUG” for many infections, and we should all be humble enough to accept it. Patience and trust in your treatment can go a long way to treat the infection as well as restrict the spread of AMR.
Conclusion
Anti-microbials are our sacred weapon towards saving lives, but only if we use them judiciously. Anti-microbials can help save lives, but only if we use them for that purpose only, under the hands of experts trained to use them judiciously. Hence, the next time you feel you have an infection, please visit your doctor, and not the pharmacy store to buy anti-microbials, as chances are it may not need any anti-microbial therapy!
Paras Pathology has been offering automated culture and sensitivity testing of blood, stool, sputum, urine, etc. with standardized reporting for bacteria and fungi, according to the latest CLSI guidelines. We are one of the few labs conducting microbiology testing with NABH certification of quality services. For more information on the tests and packages, please visit www.paraspathology.com or call 7045280906. Please feel free to write to us at info@paraspathology.com if you have any suggestions / queries regarding the information given in this blog.
.
Keywords : AMR, Antibiotics, Antimicrobials, WAAW
Authors: Dr. Munjal Shah, MBBS, MD (Pathology)
Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
The COVID-19 pandemic is thankfully receding, however, it seems our old enemy is back! The city is seeing a significant rise in dengue cases in recent times. With the break we got from dengue last year, it would be worthwhile to go through the CBC and peripheral smear changes.
How does CBC and peripheral smear help in Dengue cases?
Common Practical Terms, and their explanations
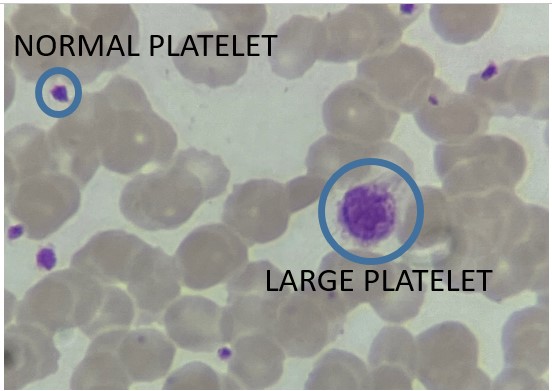
The term “IPF” or “Immature Platelet Fraction” is actually a misnomer, as there are no immature platelets in circulation! IPF is a machine related term, which translates to larger sized and more granular platelets in circulation. During episodes of thrombocytopenia due to any cause, the bone marrow compensates the platelet deficiency state by throwing out the platelets early, hence their large size. Read on to find out more!
Other common “machine related” term is High Fluorescent Lymphocyte Count, abbreviated as HFLC. These are nothing but reactive lymphocytes, as explained below.
Natural History of Dengue Infection, from CBC perspective
Let us now understand how the functions mentioned above are fulfilled by understanding the changes in CBC and peripheral smear during the course of dengue infection.
Dengue infection usually starts with high grade fever with our without headache, joint pain, myalgia, etc. As per tradition, we usually count the days from the first of symptoms. All CBC and peripheral smear parameters are explained from this day onwards.
First day is usually the day of high fever with a toxic (sick) look. The CBC shows normal WBC count, with a neutrophilic differential and gradually developing eosinopenia (low eosinophil). It must be noted that neutrophilic differential and eosinopenia are hallmarks of early phase of any infection. Eosinopenia usually persists untill resolution of the infection, about 7 to 10 days, while for viral infections like dengue, the neutrophilic differential continues only until day 2 or 3.
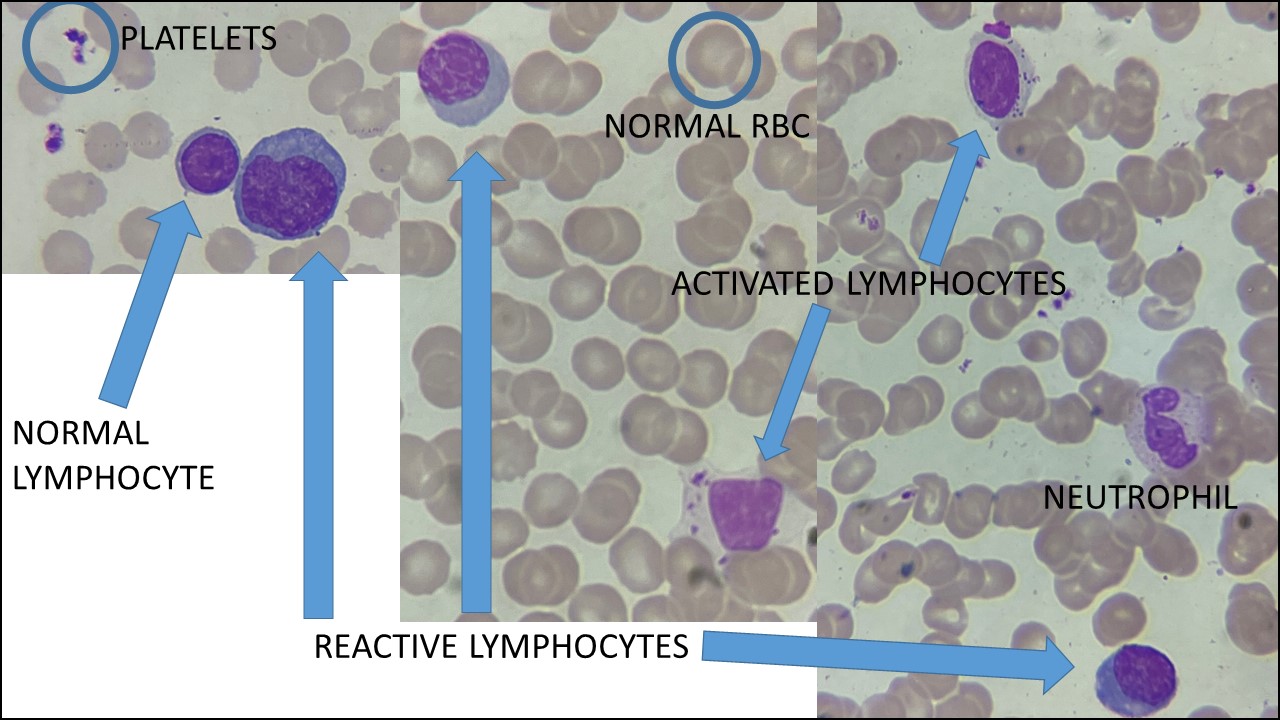
From the second or third day, an early sign of dengue infection seen as leukopenia (fall in the total WBC count). This is followed by normalising differential count, and presence of activated lymphocytes in the peripheral smear. By approximately the fifth day, the differential count becomes lymphocytic, and you can start seeing reactive lymphocytes in the peripheral smear. Reactive lymphocytes are transformed B-lymphocytes full of antibodies against a virus, or any particular antigen. They are usually larger than a normal lymphocyte. Reactive lymphocytes are also called “blue plasma cells” or just “plasma cells”. Another type of lymphocytes are "activated lymphocytes" or large granular lymphocytes. These are usually Natural Killer "NK" cells, which act as first line of defence against viral infections, before reactive lymphocytes are formed. All these types of cells are seen in the picture given below at the same magnification for size comparison, please note the difference in size and appearance amongst each type of lymphocyte.
From the third to fifth day, the platelet count starts falling. This usually coincides with most patients becoming asymptomatic, that is, fever and other symptoms reduce significantly or completely disappear. Due to the sense of well-being, patients tend to become more complacent. They must be educated to keep a watch on falling platelets and rising hemoglobin and hematocrit. Rise in hemoglobin or hematocrit is due to hemoconcentration, caused by the shifting of intravascular fluid into the interstitial compartment facilitated by reduction in number of platelets.
The rate and extent of fall of platelets is difficult to predict, hence CBC with peripheral smear plays a vital role here. Using the peripheral smear, we can predict when this fall will cease, or when we can expect a rise. The two signs which we look at are presence of reactive lymphocytes and large platelets. Large platelets is a microscopic term given to platelets when their size almost approaches the size of RBCs (See pic below). IPF mentioned by machines is nothing but presence of large platelets. Thus, a good microscopic exam is all you need! In our experience, presence of large platelets and reactive lymphocytes gives an assurance that platelet counts shall stop falling and/or increase within the next 24 to 48 hours. Increase in platelet count is confirmed by a CBC on the following day, and that is usually considered the start of the recovery phase!
Serological Diagnosis
The NS1 antigen usually comes positive within first three to five days of symptoms. From about the fifth to seventh day of symptoms, IgM antibodies start showing up, and thus this test comes positive. Notice from above discussion, that this period coincides with the presence of reactive lymphocytes. Thus, first three days warrant investigating with NS1 antigen, and beyond seven days it would be advisable to investigate with IgM antibody only. The middle period is the “conversion period” so better to investigate with both. Finally, IgG antibodies to dengue are seen after approximately 10 to 14 days of infection, and thus have a limited role in diagnosing acute infection.
Outliers: Unusual, but not uncommon occurences
Some patients maintain normal platelet count throughout the illness. On the other hand, in some cases, platelet count tends to drop drastically and very early in the infection, such that it appears to do so along with fall in total WBC count.
Conclusion:
Although we discussed a lot of features in CBC and peripheral smear, please remember that none of these are exclusively seen in dengue infection. Many of these features are described in most viral infections. However, during monsoon when mosquito breeding is at its peak, and when dengue cases are on the rise, and in the absence of serological diagnosis, a patient showing above features may fairly point to a possibility of dengue infection, and must be investigated accordingly.
We would love to hear from you! Please send your comments/suggestions/criticism about this article to info@paraspathology.com and we will be happy to read them!
Disclaimer: The intent of this article is to educate the reader (a medical professional) with certain common points in a dengue virus infection. The points mentioned above are through the experience of the authors as seen in many dengue cases over the years. An individual case may deviate from the common points mentioned here and hence all clinical factors should be taken into consideration before taking a clinical decision. The authors take no responsibility of the same. Also, the timelines given in this article are a general guideline based on the experience of the authors, but can vary to any extent in an individual case.
Keywords : Dengue, CBC, Peripheral smear
Authors: Dr. Munjal Shah, MBBS, MD (Pathology)
Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Blood sugar testing is the most common test for any medical laboratory, and unfortunately, also the most misunderstood one. Sugar test is basically testing “glucose” which is the most preferred substance for all our body cells’ energy needs.
The most common reason for sugar testing is either to screen for diabetes in a patient or to understand the control of sugar levels in a known diabetic patient. There are many other reasons for looking at blood sugar levels but enlisting all is beyond the scope of this article. If you are a diabetic, then you might be frequently testing your sugar at home. Regular testing in a quality certified laboratory is advised to make sure that your home device readings are correct. In non-diabetic individuals, blood sugar levels are also advised as a baseline investigation to anyone above the age of 30 years.
Following is the summary of the most common blood sugar tests and their significance… (covering all tests is beyond the scope of this article, you can check the names of few other tests under our “diabetic profile”)
1. Fasting Blood Sugar
Here, “fasting” usually refers to overnight fasting, which in numerical terms refers to 8 hours fasting during which no foods or liquids should be consumed. However, a common misconception is not drinking water! Please remember that plain water CAN BE CONSUMED during this fasting period, so make sure you are hydrated, especially during summers! This test is commonly abbreviated as BSF or FBS, where B stands for Blood, F for Fasting and S for Sugar.
2. Post Prandial (PP) Blood Sugar
This test is probably the most misunderstood one. The literal meaning of the term “prandial” is “meal”, so while giving post prandial blood sample, it is important to note whether this is post breakfast, post lunch, or post dinner testing. This is very important, as most patients assume this test as “post-lunch” but end up giving a “post-breakfast” sample, calling it a “heavy breakfast”. The post prandial blood sugar assesses the body’s response to a meal, so it is important to classify which meal it is, and thus, if you are a diabetic, your therapy schedule will be decided accordingly. For the same reason, it is also important to test your post prandial sugar as part of your daily routine and not make special changes to your meal routine or your medicines during the day of the test. At Paras Pathology, we ask the patient if it is a post breakfast or post lunch sample. If it is post breakfast, we shall mention that in our report, as post prandial is usually assumed to be post-lunch sample. Another point to understand here is whether testing at home or at the laboratory, 2 hours should always be counted from the START of the meal. Common mistake done is counting 2 hours after ending the meal, which leads to errors as everyone takes different amount of time to finish a meal. Once your meal is over, please do not have anything except plain water until your blood sample is collected. Post prandial sugar is abbreviated as BSPP, PPBS and rarely as PLBS, where PP stands for Post prandial, and PL for Post lunch.
3. Random Blood Sugar
This is the most convenient form of sugar testing as this test can be taken at any time of the day irrespective of the patients fasting or non-fasting status. This is usually advised as a screening test in an otherwise non-diabetic patient, or as an emergency test in a sick patient. It is usually abbreviated as RBS or BSR, where R stands for Random.
4. Urine sugar
Historically, this test was used to diagnose diabetes, but that concept is now outdated. This is mainly due to the advancement in blood sugar testing, and the inaccuracy of urine sugar in reflecting blood sugar. Normal urine doesn’t show sugar, however, if the blood sugar levels rise above a particular level, called “renal threshold”, then we see sugar in urine. However, it is now understood that renal threshold is different for every individual depending on age, gender, and other diseases. If someone has damaged kidneys, renal threshold will be so low, that even with normal blood sugar, there can be sugar in urine, thus raising false alarms. Additionally, recent advances in medical therapies have led to the development of certain tablets which act by deliberately pushing sugar into urine, thus rendering urine sugar tests totally unreliable.
5. Glycated haemoglobin (HbA1c)
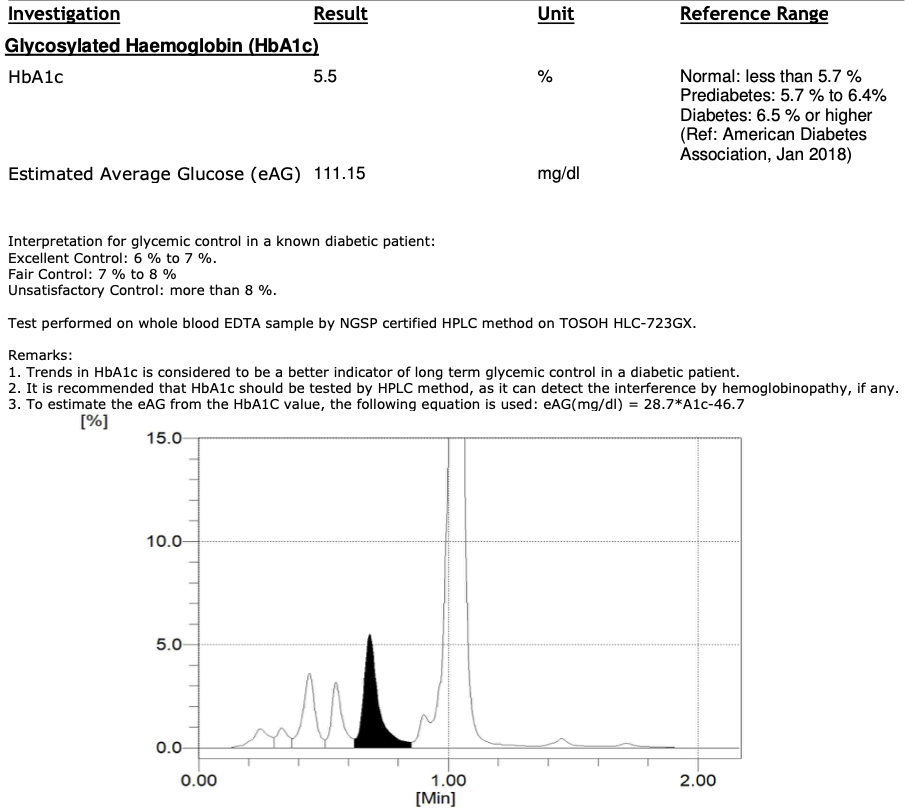
This has emerged as one of the most reliable parameters in diagnosis of diabetes in a new patient, and also understand the sugar control in a known diabetic, as it does not get significantly affected by any short temporary change in body functions like an infection, unlike blood sugar levels. HbA1c is a parameter which reflects the blood sugar over the last three months, with most weightage from the last one month. This test also doesn’t need a fasting state, which also adds to the convenience factor. However, a critical factor in reliability of this test, is to do this test by HPLC method only, which is globally considered as the gold standard method for HbA1c testing. This is for two reasons: first, HPLC gives a very accurate result and second, HPLC also detects haemoglobin variants, which may interfere with HbA1c results. No other HbA1c method has these advantages, and hence, testing by HPLC method must be insisted. For this reason, Paras Pathology tests HbA1c only with HPLC method, and we print the graph on the report for authenticity, as seen in the picture below.
Notes on Interpretation of your blood sugar report
1. A popular misconception is that post prandial sugar should always be higher than fasting blood sugar. However, there are two very common reasons where post prandial blood sugar is less than fasting sugar as given below:
a. This is most commonly seen in diabetic patients and is usually associated with taking your anti-diabetic tablet around the meal after which blood sample was collected.
b. In some normal individuals, this can be seen as a result of an exaggerated body’s response to your meal. This is medically termed as “hyperinsulinemic response”.
2. Blood Sugar results can get affected by current disease, treatment with certain medicines, sudden changes in diet, etc. Hence, these results should always be discussed with your family doctor or treating doctor.
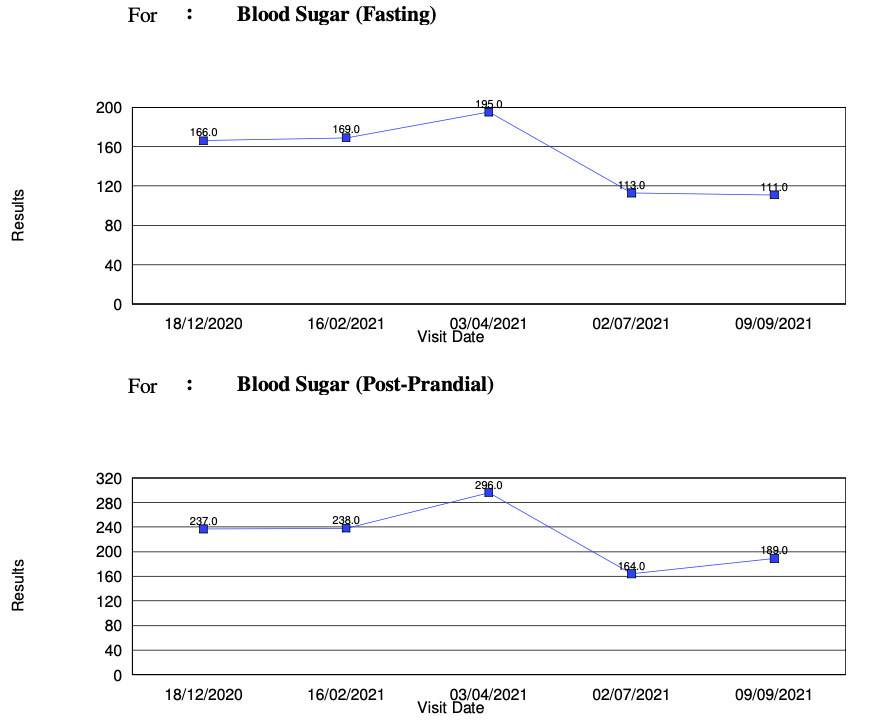
3. Since daily blood sugar levels can be very easily affected by many factors, it is worthwhile to understand the “trend” of results rather than individual values. Paras Pathology offers such a “trend analysis” to all its regular patients. This basically gives a graphical analysis of your last five sugar reports done with us as seen in the picture below.
Conclusion and Take-Home messages
1. For fasting blood sugar, eight hours fasting is a must, only plain water can be consumed during this period.
2. For fasting and post prandial blood sugar test, do not change your daily routine on the day of the test. The tests should be accommodated within your daily routine of meals and diabetic medications for getting the best reflection of your blood sugar levels.
3. If your doctor prescribes you the post prandial test, please discuss the timing of your post prandial test, whether it should be post-breakfast, post-lunch or post-dinner with your doctor before giving the blood sample. At the time of giving the post prandial sample in the laboratory, kindly notify them about it whether its post-lunch, post-breakfast or post-dinner.
4. Remember to count the 2 hours from the START of the meal to give your post prandial blood sample, and once your meal is over, no more eating until sample is given, except plain water.
5. It is possible to have post prandial sugar lower than your fasting sugar levels.
6. Single HbA1c result is more powerful than a single fasting, post prandial or random blood sugar test, provided the HbA1c result has been done by HPLC method.
7. Single abnormal fasting or post prandial blood sugar test doesn’t mean you have diabetes, a trend analysis gives much better information. Please discuss the same with your family doctor or your treating doctor.
8. Urine sugar testing is now outdated, unless for only very specific reasons.
9. If you are checking your blood sugar at home on a regular basis, it is important to check the same periodically at a quality certified laboratory, to ensure your home device is functioning optimally. If the results do not matchm then it is time to change or repair your home device!
We thank Dr. Nilesh Mali for suggesting us to write on this topic. For any suggestions/criticisms to this article, or if you want to suggest us a topic, please feel free to connect with us on info@paraspathology.com .
References
1. ICMR Guidelines for Management of Type 2 Diabetes.
2. Standards of Medical Care in Diabetes, American Diabetes Association.
Keywords : Blood sugar testing, Diabetes, glucose, sugar
Authors: Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Dr. Munjal Shah, MBBS, MD (Pathology)
You may be wondering why we have a World Mosquito Day when these insects are responsible for the transmission of malaria, and many other diseases. Well, that is what this day is all about: raising awareness about the disease spread by mosquitoes! It is also important to recognize that all the living beings on this planet play an important role in the circle of life, whether they are harmless, harmful, helpful or none of the above!
Did you know???
We, at Paras Pathology, and almost all medical practitioners and laboratories across Mumbai, saw a sharp decline in cases of malaria and especially dengue (diseases spread by mosquitoes) during monsoon of year 2020, attributed mainly to lockdown measures, which probably meant better sanitation and clean environment. This year, with decreasing lockdown restrictions, we have all started to see a sharp rise in cases of malaria and dengue. Read on to find out more on diseases spread by mosquitoes and how can we be safe…
History of world Mosquito day
World Mosquito Day is observed on 20th August every year. On this day, Sir Ronald Ross, a British doctor, discovered that the female mosquito transmits malaria between humans, way back in 1897. Malaria is a life-threatening disease. After Sir Ronald Ross made this discovery, he received the Nobel Prize in Medicine.
Mosquitoes might look small but they can KILL!
A small puddle of stagnant water causes mosquito breeding, leading to an infestation in that area, causing diseases. According to WHO, malaria causes an estimated 219 million cases globally and results in more than 400,000 deaths every year. On the other hand, dengue is responsible for almost 96 million symptomatic cases and an estimated 40,000 deaths every year. Apart from malaria and dengue Mosquito can spread many other diseases, following is a detailed list:
1) Malaria
2) Dengue
3) Chikungunya
4) Filariasis
6) Tularemia
7) Yellow fever
8) Zika fever
12) Western equine encephalitis
13) Eastern equine encephalitis
14) Venezuelan equine encephalitis
15) Ross River fever
18) Keystone virus
And list can go on… So from above list you must have understood why is it so important to control mosquito breeding and prevention from mosquito bites.
Importance of World Mosquito Day 2021:
World Mosquito day is celebrated to create awareness about mosquito borne diseases. Authorities, NGOs, etc. celebrate by providing nets, distributing information about the precautions people should take, cleaning stagnant water in your nearby area, doing pest control in your house and offices. The general public needs to be educated about healthy living habits and simple ways to avoid mosquito breeding around their homes.
The theme for World Mosquito Day 2021 is 'Reaching the zero malaria target'.
How to Prevent Diseases caused by mosquitos?
During the monsoon, a steep rise in mosquito-borne diseases is observed every year. Stagnant water acts as a breeding ground for mosquitoes. The hot and humid climate of Mumbai also accelerate mosquito breeding. Therefore, it is crucial to follow all necessary steps to prevent mosquito bites, especially during the monsoon season. Here are some tips that can help you prevent mosquito bites.
1. Choose right clothing: Wearing full-sleeved, loose clothes can help prevent mosquito bites. Avoid wearing body-hugging clothes as these allow mosquitoes to bite easily.
2. Use repellent: You can use insect spray at home to avoid mosquito bites. To naturally repel mosquitoes, try mosquito-repelling plants such as lemon balm, basil, lavender and rosemary.
3. Mosquito nets: These cause a physical barrier, and useful for open spaces, where repellants wont work.
4. Keep surroundings clean: Do not allow water to collect in your garden or places near you. Keep containers, pots, buckets and other containers upside down to prevent unnecessary accumulation of stagnant water. Introducing larvivorous (mosquito larvae eating) fishes in ornamental water tanks/gardens or nearby ponds can help prevent mosquito breeding. In urban areas where construction work is on, you can call in B.M.C Pest control department on 022 2201 4022 (for Mumbai) to help control mosquito breeding.
Watch out for symptoms
Mosquito-borne diseases are common during monsoon. Common symptom of mosquito borne diseases are fever, tiredness, vomiting, headache etc. There are specifics tests to diagnose each of these diseases. If you experience any of the symptoms mentioned above in the monsoon season, seek medical help immediately through your family doctor, and may prescribe some particular tests depending on clinical judgement. For details on the tests prescribed to you contact us on 7045280906.
This World Mosquito Day, take note of these tips and safeguard yourself and your family.
Keywords : Mosquito, Monsoon, Fever
Authors: Dr. Munjal Shah, MBBS, MD (Pathology)
Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Lipid Profile is one of the most common tests, especially in the preventive health domain. It is recommended to test your lipid profile in men after the age of 35 years, and periodically every 6 to 12 months (1, 2). And many seem to be doing it… however, few of them understand the report, in its entirety. Here, we describe the lipid profile as it should be understood from the perspective of the patient.
What is the importance of testing my Lipid profile?
Cardiovascular disease is emerging to be one of the common reasons for death and disability. Recent trends indicate, these diseases are no longer limited to elderly, and are seen affecting the relatively younger population also. One of the most important and modifiable risk factors in determining the possibility of cardiovascular disease in an individual person is the status of their lipid profile (3). Keeping the lipid profile in check has shown to prevent possible cardiac events in a patient, and also restrict the progression of blockage or clogging their arteries. (3).
Thus, lipid profile forms one of the simplest, cost effective, and first line investigations in the work-up of a patient to determine the risk of cardiovascular disease.
How do I prepare for taking the test?
The usual recommendation is a minimum of 12 hour fasting period, during which drinking water is permitted without any additives.
A new concept of non-fasting lipid profile has recently gained some attention, due to the difficulties involved with maintaining a strict minimum 12 hour fasting period. However, in case of an abnormal result, it is difficult to standardize the readings with the meal taken which is variable based on a person’s diet, and hence would invariably entail the patient to undergo the fasting test. Also, all the guidelines related to treatment of hyperlipidemia are standardized based on the results of a fasting lipid profile (3, 4).
Paras Pathology recommends its patients to have a strict minimum 12-hour fasting period to ensure the reproducible and comprehensible results.
How is my sample collected?
Sample collection for a lipid profile is in the usual manner, as for all blood tests. At Paras Pathology, sample for lipid profile is currently collected in a red capped tube, to which a label is attached bearing the patients details and a unique bar code.
What is tested?
A lipid test is called a profile because of the variety of parameters covered as given below (picture shows an example of our new report format):
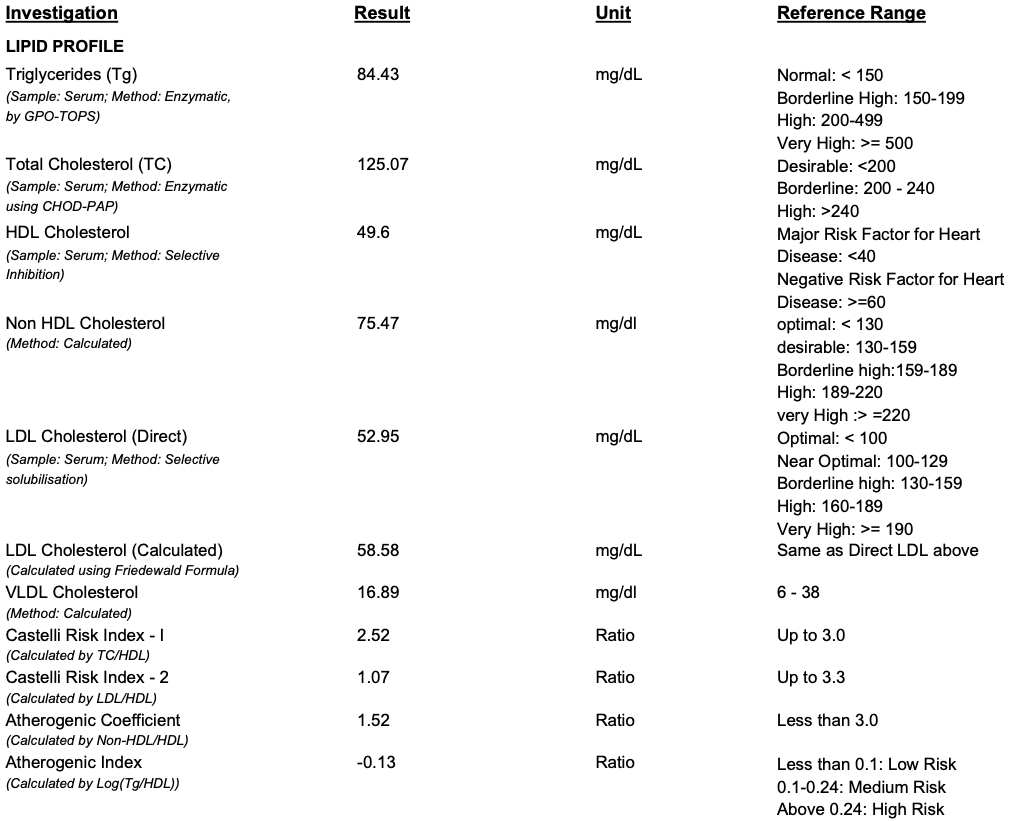
A. Triglycerides: After a meal, most of the fatty foods get converted to triglycerides, which are carried in the form of chylomicrons. In case of a heavy fatty last meal, or in case a patient doesn’t observe the recommended 12-hour fasting, this parameter is the most affected. As this parameter is directly affected by the immediately recent diet, this parameter may show the large variations in the same person in a matter of days. In the laboratory, this parameter is directly measured from the collected blood sample. High triglycerides is also target for cholesterol treatment, after LDL (3).
B. Total Cholesterol: This represents all forms of cholesterol present in your blood (different cholesterols described below, that is, HDL, LDL and VLDL). In theory, this value is the sum of all the different types of cholesterols. In the laboratory, this parameter is also directly measured.
C. HDL Cholesterol: This is commonly known as the “GOOD” cholesterol, as this is involved in “reverse cholesterol transport”, that is, it transports cholesterol from different parts of the body into the liver, for body function, thus helping in utilizing the cholesterol. As this REDUCES the cholesterol burden in the body, it is considered “good”, therefore, higher the HDL, lower the chances of health risk. This parameter too, is directly measured in almost all laboratories when you order a lipid profile.
D. LDL Cholesterol: This is commonly known as the “BAD” cholesterol, as this is type of cholesterol transports cholesterol from the liver to different parts of the body causing deposition of cholesterol at various unwanted places, like in our arteries, leading to the side effects of cholesterol, that is, clogging of the arteries (called “heart attack” when this happens in the heart, and “stroke” or “paralysis” when it happens in the brain).
This parameter is reported in two ways. Most laboratories report this parameter by calculation, using “Friedewald equation”, which gives a fairly good estimate, without having to directly measure this parameter. This helps in reducing the testing cost. However, as this equation uses triglycerides to estimate LDL, calculated LDL will also reflect the variations seen in triglycerides, which forms a disadvantage of using calculated LDL. Also, there studies also indicate that in many instances, the calculated LDL cholesterol may be over or underestimated as compared to the directly measured result (5, 6). There are multiple studies favoring direct measurement of LDL cholesterol, rather than from the formula, as LDL is the primary target of cholesterol lowering therapies (3). Hence, there are few laboratories that do measure this parameter directly, thus giving a precise value, rather than an estimate derived from a formula, but increases the cost of testing.
As LDL may be considered the single most important parameter in the lipid profile to be monitored, Paras Pathology has always reported directly measured LDL, and recently, we have started reporting both the directly measured as well as the calculated values (see attached picture)!
E. Non-HDL Cholesterol: Since most laboratories do not measure LDL directly, using non-HDL as a surrogate marker eliminates the variations of calculated LDL, as this parameter uses only total cholesterol and HDL cholesterol, both of which are relatively stable parameters over time. Thus, it is also considered a secondary target of therapy (3).
F. VLDL Cholesterol: This is the last type of clinically significant cholesterol that is reported. They are temporary molecules, formed during the process of lipid metabolism. VLDL result is always calculated from triglycerides.
G. Lipid Ratios: As our understanding of the lipid metabolism increased, scientists and doctors believed that, although the individual results are important, even when these are normal, some patients still ended up with some cardiovascular issues. This brought up the concept of “lipid ratios”, which are derived from more than one lipid parameter. The list of ratios are as given below:
a. Castelli Risk Index 1
b. Castelli Risk Index 2
c. Atherogenic coefficient
d. Atherogenic Index
Amongst the ratios mentioned above, the first two ratios, that is, the Castelli Index 1 & 2 are most commonly reported in almost all laboratories. In a given patient, a ratio can be abnormal, even though all cholesterol values are normal. Thus, the ratios are developed to help in better understanding the effects of all the different cholesterols, even when they are apparently normal. Hence, Paras Pathology reports all 4 types of ratios in its lipid profile report, as each have a significance, based on a particular patient profile.
Conclusion
Lipid profile forms one of the simplest, cost-effective, and one of the first line investigations in determining the cardiac risk of a patient. The entire test gives a lot of information, but that needs some basic understanding. Overall, the target is to reduce the “Bad” LDL cholesterol and keep the “Good” HDL cholesterol at a higher level. A directly measured LDL cholesterol should be preferred.
References
1. Wander, G.S., Jadhav, U.M., Chemburkar, A. et al. Lipid management in India: a nationwide, cross-sectional physician survey. Lipids Health Dis 16, 130 (2017).
2. Screening for Lipid Disorders in Adults: Recommendation Statement. Am Fam Physician. 2009 Dec 1;80(11):1273-1274.
3. Bethesda, et al. National Cholesterol Education Program. ATP III Guidelines at-a-Glance Quick Desk Reference, 2001.
4. Nigam PK. Serum Lipid Profile: Fasting or Non-fasting?. Indian J Clin Biochem. 2011;26(1):96-97.
5. Lindsey, C.C., Graham, M.R., Johnston, T.P., Kiroff, C.G. and Freshley, A. (2004), A Clinical Comparison of Calculated versus Direct Measurement of Low-Density Lipoprotein Cholesterol Level. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 24: 167-172.
6. Kannan S, Mahadevan S, Ramji B, Jayapaul M, Kumaravel V. LDL-cholesterol: Friedewald calculated versus direct measurement-study from a large Indian laboratory database. Indian J Endocrinol Metab. 2014;18(4):502-504.
Keywords : Cholesterol, Lipid Profile, Blood Tests, Pathology
Authors: Dr. Munjal Shah, MBBS, MD (Pathology)
Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Did you know?
As COVID-19 is a new disease, there is no “standard” levels of antibodies established which can be considered “protective” against COVID-19 infection. This is mainly because until recently, there was no standardised unit for measuring antibody level. With the recent announcement by WHO of a “standardised unit” of antibody measurement (1), we can expect a “truly quantitative” antibody test to be available soon! And hopefully, a “protective” antibody level will be established soon!
Read on to find out more…
What is Antibody?
Antibody is a protein developed by our body’s immune system to fight foreign particles entering our body. These foreign particles maybe bacteria, viruses, parasites, allergens, etc. The body can produce 5 types of antibodies in total, called immunoglobulins (abbreviated as “Ig”), each having their own significance as follows:
1. Immunoglobulin G (IgG): This is the most abundant form of antibody in blood and is associated with long term immunity, as this antibody is produced by the body for the longest period of time.
2. Immunoglobulin M (IgM): This is the largest antibody produced and is usually the first antibody produced in the blood against the foreign body. However, its quantity decreases within a few weeks, as IgG response starts increasing.
3. Immunoglobulin A (IgA): This is related to “local” or “membrane” immunity, like that of our mouth, nose, digestive system, etc. Its levels are relatively low in the blood as compared to IgG and IgM.
4. Immunoglobulin D (IgD): This is the rarest form of antibody found in our body, and its exact function is also not known.
5. Immunoglobulin E (IgE): This antibody is related to allergic reactions, so not relevant in this discussion.
The usual response of our body to any foreign agent or microbe is IgA at the point of entry (nose, mouth, etc), IgM in blood within a few days up to a few weeks, and finally IgG in blood, starting from a few weeks, until months, years, or even for life. Thus, in terms of measuring antibody levels in blood, practically, the levels of IgM and IgG are only relevant as far as COVID-19 is concerned.
What is the Antibody against COVID-19?
As COVID-19 is caused by a virus (called SARS-CoV-2), the body develops antibodies against this virus. However, the body doesn’t produce antibody against the virus as a whole. It produces antibodies against particular parts of the virus, called “antigens”. These antigens are part of the proteins which form the virus. Studies have shown that the SARS-CoV-2 virus has four important proteins: Nucleocapsid protein, Spike protein, Membrane protein, Envelope protein, abbreviated as N, S, M & E protein respectively. Antibodies can be formed against all these proteins by our body, when the virus enters our body. As the virus latches onto our body using the S protein, antibodies against the S protein are sometimes called “neutralising” antibodies (2), as these antibodies prevent the virus from entering our body, thus reducing its effects on our body.
COVID-19 Antibody Test… What is tested?
As seen above, our body produces antibody against 4 parts of the virus, out of which we largely test for either the antibody against N protein or S protein or both. Also, antibodies against these proteins can be of IgG, IgM or IgA type. therefore, if infected by the SARS-CoV-2, our body can have 6 types of antibodies which can be tested, that is, IgG, IgM, and IgA against N protein and IgG, IgM, and IgA against S protein. When we test for all these antibodies, we call it "Total Antibody Test". The total antibody test can test for antibodies against S protein or N protein or both.
Another specific test can be testing for IgG, since for all practical purposes, this is our long-lasting antibody (as described above). Tests can be for IgG against S protein or for N protein or for both (sometimes called “Total IgG”). Theoretically speaking, as this antibody provides long lasting “immunity” and is also the most abundant antibody in blood, it is more practical to test for this antibody.
A rather unpopular antibody test is testing for IgM antibody. For most infections, like in dengue virus, IgM antibody to virus comes first. Within a few weeks, this IgM is completely replaced by IgG. However, in COVID-19 infection, it has been observed that IgM and IgG are produced almost simultaneously (gap of two to four days only) (3), thus reducing the importance of IgM testing.
Therefore, in short, you can test for Total antibody, or IgM antibody or IgG antibody. These antibody tests can be against either S protein or N protein or both. So all antibody tests would be some permutation or combination of these variables.
Which Method of Antibody Testing to choose?
There are three methods of testing COVID-19 antibodies:
· Qualitative: The result is given as positive or negative, based on comparison with a known standard concentration. Thus, these tests are reported as “ratio” or “index” to the known standard. (The number given with qualitative antibody test reports is the strength of the signal against the known standard). At PARAS PATHOLOGY, we have been testing IgG antibody against spike protein in qualitative manner since September 2020 upto July, 2021.
· Semi-quantitative: These tests give an approximate titre based on their calibration, but the reporting units are “arbitrary”, that is, in simple language, “assumed” and are thus reported in Arbitrary Units per mL, abbreviated as AU/mL. As semi-quantitative tests are, in other words, “partially quantitative”, they may be used to get “quantitative” results using a conversion factor.
· Quantitative: A recent publication from the WHO has standardised the antibody testing in units of “BAU/mL” (BAU stands for Binding Antibody Units) (1). Thus, “truly quantitative” COVID-19 antibody tests would give the report directly in this units, without using a conversion factor. Since this concept is relatively new, these are still not commercially available.
Another hybrid manner of antibody testing is using the ratio of qualitative testing and equating it with quantitative data to determine its corresponding quantitative antibody value. This enable reporting the antibody results in a quantitative manner, based on the WHO standard as stated above, that is, BAU/mL. Since, this method is also not "truly quantitative", it can be put under "semi-quantitative" category.
Paras Pathology has started testing with this method, as until the "truly quantitative" tests are available commercially, we feel this is the closest we can get to quantitative results.
When to get tested?
If you had a COVID-19 infection, you are likely to have antibodies against the virus 14 days after the onset of symptoms. You can test for any of the antibody tests mentioned above, all of them should come positive. As the time between the onset of symptoms, and date of testing increases, your body will have increasing dominance of IgG antibody, and thus, testing for IgM would be negative. In our experience of testing for COVID-19 IgG at PARAS PATHOLOGY, we have noticed that stronger the symptoms of COVID19, higher is the antibody response. However, we have also noted that these antibody levels tend to decrease over time.
A scientific paper published in The Lancet in April, 2021, mentions that COVID-19 antibody lasts for up to 10 months. The study also found that young individuals maintained the antibodies for a longer time than those above 65 years of age. It also mentioned that antibody against N protein decreased faster than that against S protein. (4).
Antibody Test after vaccination… Which one to choose?
In India, there are two types of vaccines available: COVISHIELD and COVAXIN. Any antibody response in our body, is usually studied after 14 days of exposure. Hence, the results given below are seen after atleast 14 days of second dose of each vaccine.
COVISHIELD is a vaccine made by injecting the S protein of SARS-CoV-2 into another virus. Thus, antibody tests after both doses of COVISHIELD will be positive for IgG against the S protein, but a total antibody test or IgG test against N protein will be negative.
COVAXIN is made using a killed SARS-CoV-2. Hence, when you get the shot of this vaccine, you are essentially getting all the proteins of COVID-19 infection, but not the disease. Hence, the antibody test results will be similar to that of COVID-19 patient, that is, positive for all IgG, IgM and total antibody tests.
|
Antibody test (Total or IgG) |
for COVAXIN |
for COVISHIELD |
|
Against N Protein |
Positive |
Negative |
|
Against S Protein |
Positive |
Positive |
Note: If you are trying to guage which vaccine is better based on the above facts, then please remember this: THE BEST VACCINE IS THE ONE WHICH REACHES YOUR ARM FIRST!
Interpretation of COVID-19 Antibody test
Following table is a short summary to interpret the COVID-19 antibody test:
|
N Protein |
S Protein |
Interpretation |
|
Positive |
Positive |
Patient has either taken COVAXIN vaccination or had COVID-19 infection in recent past |
|
Positive |
Negative |
Not seen yet, unlikely results |
|
Negative |
Positive |
Patient has taken COVISHIELD vaccination in the recent past |
|
Negative |
Negative |
No history of vaccination or COVID-19 infection, in the recent past. However, this result may be seen in some infected, and/or vaccinated individuals, due to various patient and test related reasons. |
Conclusion
This blog is intended TO EDUCATE the patient about the COVID-19 ANTIBODY TEST. As COVID-19 is a novel disease with much ongoing research, many facts and information presented here may change as we understand this disease better. We shall continue to modify this blog as and when such information is made available, so we can provide you with updated information. Currently, PARAS PATHOLOGY performs the the semi-quantitative IgG Antibody test against the Receptor binding domain of the spike protein of COVID-19 virus, as we believe that this antibody provides the best results applicable in the current scenario (based on the discussion above). However, as newer methodology would be available, PARAS PATHOLOGY would be enthusiastic to adopt the same!
Note: Although the antibody seen in COVID-19 is reported as “Anti-SARS-CoV-2 Antibody”, which is its true scientific name, for the purpose of simplicity in this blog, we called it “COVID-19 antibody”.
References
1. Kristiansen PA, et al. WHO International Standard for anti-SAR-CoV-2 immunoglobulin. Vol 397; Issue 10282, 1347-8. Link to Article
2. S. Xiaojie, L. Yu, Y. Lei, Y. Guang, Q. Min. Neutralizing antibodies targeting SARS-CoV-2 spike protein. Stem Cell Res., 50 (2020), p. 102125. Link to Article
3. CDC Website https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests-guidelines.html
4. D. Alfego et al., A population-based analysis of the longevity of SARS-CoV-2 antibody seropositivity in the United States, EClinicalMedicine (2021). Link to Article
Keywords : COVID-19, Anti-SARS-CoV-2, Antibody, IgG
Authors: Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Dr. Munjal Shah, MBBS, MD (Pathology)
Did you know???
Traditionally, the term “Black Fungus” is used for Phaeoid (dematiaceous) fungi in medical microbiology due to its brownish black color on a KOH mount under the microscope. In fact, the term “Phaeoid” literally means “dark” as these fungi contain melanin.
Thus, mucormycosis isn’t really the “black fungus”, however, it does give black color on the area where it grows, leading to this misunderstanding. The black color here isn’t from the fungus itself, but from the dead “necrotic” tissue as a result of the fungal infection.
Read on to know more….
Background
Mucor is a fungus commonly found in plants, soil, decaying fruits and vegetables. It is also found in air and dirt and may even be found in the nose and mouth of healthy individuals, without causing any infection.
Mucor usually enters the body through inhalation while breathing, ingestion from mouth or injection through skin. It can affect any part of the body, and the disease caused in the human body due mucor is called “mucormycosis”.
Mucor & Mucormycosis
Mucor has been known to cause disease in humans since 1855. Mucormycosis is the term given to the infection and disease caused by mucor in humans. It is an “opportunistic infection”, that is, it typically affects people with a weak immune system like patients of HIV/AIDS, diabetes, cancer, long standing steroid therapy, etc. Healthy individuals may unknowingly harbor the fungus on their body without actually suffering from the disease.
Mucor is notorious for entering the blood vessels (also called angio-invasive) and rapidly destroying body tissues. Thus, mucormycosis becomes a medical emergency.
COVID-19 & Rise of Mucormycosis
COVID-19 makes a particularly suitable environment for mucor to cause disease through the following three ways:
1. Steroids are used in COVID-19 treatment to tackle the “cytokine storm” which is basically our immune system in overdrive. Steroid treatment help by suppressing the immune system, in turn allowing entry to mucor, due to the weakened immune system.
2. High blood sugar levels (hyperglycemia) help mucor to grow (Mucor seems to have a sweet tooth!). Hyperglycemia is seen in COVID-19 patients if the patient has pre-existing diabetes, and also due to the use of steroids.
3. Humidifier is used during oxygen therapy. And we all have experienced fungus and its love for moisture! (Remember the moistened bread experiment in school?)
In presence of one or all these three factors, in COVID-19 patients, mucormycosis usually starts as a black patch in the mouth or nose, and with its tissue destroying nature, may progress to the eye and may further reach the brain. Such an extensive disease may itself be life threatening, hence early diagnosis and treatment is crucial.
Laboratory Testing for Mucor
In case your are worried about this, please consult your doctor. Once your doctor examines you, any area suspicious for mucor infection can be scraped and submitted for testing. A test called “KOH mount”, available at Paras Pathology, can show a typical picture of mucor, with report in a couple of hours. If the KOH mount indicates presence of mucor then confirmatory tests like Fungal Culture and MALDI-TOF may be undertaken, but report may take a longer time.
References:
1. Jagdish Chander, “Textbook of Medical Mycology”, 4th edition, Jaypee Publications.
2. Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, Bhalla A, Puri GD, Chakrabarti A, Agarwal R. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia. 2021 May;186(2):289-298. Link to article
3. ICMR & MOHFW https://www.icmr.gov.in/pdf/covid/techdoc/Mucormycosis_ADVISORY_FROM_ICMR_In_COVID19_time.pdf
Keywords : COVID-19, Mucor, Mucormycosis, Pandemic
Author: Dr. Munjal Shah, MBBS, MD (Pathology)
Background: Viral infections are known to cause lymphocytic stimulation (1). In terms of seeing that under the microscope, we can see that as larger granular lymphocytes (LGL) activated lymphocytes and / or reactive lymphocytes. In the current context of suspected second wave of COVID19 virus, a suspicion of viral infection would culminate to considering infection with SARS-CoV-2.
Observation: I had noticed an increase in the proportion of cases showing lymphocytosis with LGLs, activated lymphocytes and / or reactive lymphocytes during the first wave of COVID-19, and i’m seeing a similar rise in such cases now, which in my opinion corresponds with the second wave. I’d like to propose that absolute and / or relative lymphocytosis, along with a microscopic picture showing LGLs, activated and / or reactive lymphocytes, can help us suspect a case of mildly symptomatic COVID-19.
Literature Search: There are very few articles on peripheral smear morphology in COVID-19, but one such article does mention the increase in variant lymphocytes in COVID-19 (2). However, these studies are usually done on hospitalised patients, which have a more severe form of disease, and thus usually report lymphopenia, and bad prognosis.
Utility: It has been established that most people having COVID-19 have a mild course (3). The advantage of having a simple parameter to raise suspicion, is to identify the mildly symptomatic patients as they may or may not seek medical opinion or may be reluctant to take the swab test, thus preventing a confirmed diagnosis. Patients with the above mentioned features should be emphasised to take the saws test. For the patient, having these changes (lymphocytosis and lymphocytic activation), may also indicate a good prognosis, as conversely, a drop in lymphocytes (lymphopenia) has been established as a bad prognostic factor (4).
Limitations: With limited follow-up due to practise constraints, it is difficult to scientifically prove this observation. Also, this observation would be irrelevant once the incidence of COVID-19 drops in the community. Lack of published data on peripheral smear study in mild cases of COVID-19 also raises concerns.
Appeal: I request all my pathology and clinical colleagues to look for lymphocytosis and lymphocyte morphology in the samples they receive in the laboratory, correlate with COVID19 test if taken in the future and share their thoughts on the observation mentioned above. A good follow-up can help us understand this observation better. Please do share any such significant findings, in support or against the above made observations.
Disclaimer: The above hypothesis does not preclude or replace the clinical judgement. However, it may aid the clinician’s diagnostic and prognostic chain of thoughts, which is the crux of laboratory medicine. These are my observations only, and not any guideline or method of practice to be followed.
References:
1. Adewoyin AS, Nwogoh B. Peripheral blood film ? a review. Ann Ib Postgrad Med. 2014;12:71?79.
2. Nazarullah et al. Peripheral Blood Examination Findings in SARS-CoV-2 Infection. Am J Clin Pathol September 2020;154:319-329.
3. WebMD Website www.webmd.com/lung/qa/what-percentage-of-covid19-cases-are-mild
4. Tavakolpour S, Rakhshandehroo T, Wei EX, Rashidian M. Lymphopenia during the COVID-19 infection: what it shows and what can be learned. Immunol Lett. 2020;225:31–32.
Reference : WebMD Website
Keywords : Lymphocyte, COVID19, SARS-CoV-2, Lymphocytosis
Author: Dr. Munjal Shah, MBBS, MD (Pathology)
“Anemia” is a condition or disease in which the hemoglobin concentration of blood falls below normal level, thus reducing the oxygen carrying capacity of the blood. WHO estimates that 42% of children younger than 5 years have anemia worldwide (1). Although iron deficiency is the most common form of nutritional anaemia in India, folate and vitamin B12 deficiencies also contribute substantially. Furthermore, folate or vitamin B12 deficiency anaemia is more prevalent in children aged more than 5 years (2).
Iron deficiency is known to cause long term negative effects in a child’s development and hence regular screening of children is recommended (3). A child or an adult with anemia shows a multitude of symptoms, however, very few of those symptoms contribute to finding the cause of anemia.
Luckily, the cause can be found out with a simple look under the microscope of the patient’s blood (called peripheral smear examination), as seen in the following case…
Eight year old girl presented to a pediatrician with complaints of nausea, abdominal discomfort and loss of appetite since a few days. On examination, there was an obvious yellow eyes (icterus) and a pale look (sign of low hemoglobin). A clinical diagnosis of hepatitis was made. Investigations were ordered, including CBC with peripheral smear exam was ordered. CBC revealed a macrocytic anemia, with a hemoglobin of 8 g/dL.
The peripheral smear examination showed classical features of Vitamin B12 / Folic acid deficiency: macrocytes, polychromasia, basophilic stippling and cabot’s rings. Thus, the patient was treated with injection of Vitamin B12 and Folic acid. The patient showed drastic improvements in all her complaints within a week. Thus, a good peripheral smear exam can help in getting to the diagnosis of low hemoglobin by revealing a common possibility of Vitamin B12 / Folic acid deficiency. Even iron deficiency anemia, has its own typical appearance under the microscope, different from that of the one described in the case above. The good thing about these diagnosis, is that they are easily treatable with injections and tablets, and the patients usually respond well to the treatment in a matter of days!
Therefore, we believe that CBC with peripheral smear examination is crucial in a case of low hemoglobin, as a good peripheral smear exam can reveal the cause of low hemoglobin in most cases. It also means that Anemia, a common yet under diagnosed disease in India, can be diagnosed easily, is easily treatable in most cases, and is also preventable in those cases! Lets resolve to beat this disease, especially in children, to enable them to have bright future!
Acknowledgements: We appreciate the follow up, feedback, and encouragement provided by Dr. Prashant Pawar (Pediatrician).
References:
1. WHO website (https://www.who.int/health-topics/anaemia#tab=tab_1) dated 20th February, 2021.
2. Sarna A Porwal A Ramesh S et al. Characterisation of the types of anaemia prevalent among children and adolescents aged 1–19 years in India: a population-based study. Lancet Child Adolesc Health. 2020; 4: 515-525.
3. Mudra Kohli-Kumar. Screening for Anemia in Children: AAP Recommendations—A Critique. Pediatrics Sep 2001, 108 (3) e56.
Reference : WHO website
Keywords : Anemia, Nutrition, Deficiency
Authors: Dr. Munjal Shah, MBBS, MD (Pathology),
Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
A natural infection of SARS-CoV-2, produces an antibody response against two types of antigens, namely, Nucleocapsid (NC) protein and Spike (S) protein. An article published in JAMA in May, 2020, states that antibodies to NC protein are more sensitive, while those to S protein are more specific and expected to be neutralising (1). There are multiple antibody tests available, which test for both or any one of these.
Vaccination against COVID19 has become the most important topic of discussion, and rightly so. With multiple types of antibody tests available, vaccinated individuals are now turning to these tests to check for their antibody response. Currently, the healthcare workers are getting the COVISHIELD Vaccine, which contains recombinant, replication-deficient chimpanzee adenovirus vector encoding the SARS-CoV-2 Spike (S) glycoprotein (2).
We received a query regarding the antibody tests to be done to check for its immune response after vaccination. This came from a healthcare worker who took the vaccination on 19th January, 2021, and took a CLIA based “Total antibody test”, on 5th February, 2021. Since the result was negative, there was an obvious inquisitiveness regarding the reason behind the negative result. Since we perform an ELFA based IgG antibody test against the Spike (S) protein of SARS-CoV-2 at our laboratory, we proposed that as the vaccine is against the spike protein, this specific test would be more appropriate. Luckily, the person came to us the very next day (6th February, 2021) for this test, and we found the result was positive for IgG antibody with the signal cut off index of 8.9.
This incident has led us to the following observations:
1. Total antibody test can be false negative after COVISHIELD.
2. IgG Response to the vaccine can be seen in 18 days.
Based on the above observations, we propose that specific IgG antibody testing to Spike protein must be encouraged, especially in post vaccinated individuals to check for their immune response to COVISHIELD vaccine. Although this incident can be considered an isolated one, we would request more vaccinated volunteers to share their experiences about this. A larger sample size may help us confirm or refute the observations made above.
Acknowledgements: We thank Dr. Darshan Parekh for having a thought provoking discussion with us, which led us to this observation.
Reference : Jama Network
Keywords : Coronavirus, COVID-19, Vaccination, Antibody Testing
Authors: Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Dr. Munjal Shah, MBBS, MD (Pathology)
Which surfaces you should prioritize for disinfection in non health care settings??
Reference : WHO Website
Keywords : Coronavirus, COVID-19, Infection Control, Discinfection, Sanitisation, Healthcare
Authors: Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Dr. Munjal Shah, MBBS, MD (Pathology)
Reference : WHO Website
Keywords : Coronavirus, COVID-19, Infection Control, Transmission