Authors: Dr. Munjal Shah, MBBS, MD (Pathology)
Dr. Nehal Mehta, MBBS, MD, DNB (Clinical Microbiology)
Lipid Profile is one of the most common tests, especially in the preventive health domain. It is recommended to test your lipid profile in men after the age of 35 years, and periodically every 6 to 12 months (1, 2). And many seem to be doing it… however, few of them understand the report, in its entirety. Here, we describe the lipid profile as it should be understood from the perspective of the patient.
What is the importance of testing my Lipid profile?
Cardiovascular disease is emerging to be one of the common reasons for death and disability. Recent trends indicate, these diseases are no longer limited to elderly, and are seen affecting the relatively younger population also. One of the most important and modifiable risk factors in determining the possibility of cardiovascular disease in an individual person is the status of their lipid profile (3). Keeping the lipid profile in check has shown to prevent possible cardiac events in a patient, and also restrict the progression of blockage or clogging their arteries. (3).
Thus, lipid profile forms one of the simplest, cost effective, and first line investigations in the work-up of a patient to determine the risk of cardiovascular disease.
How do I prepare for taking the test?
The usual recommendation is a minimum of 12 hour fasting period, during which drinking water is permitted without any additives.
A new concept of non-fasting lipid profile has recently gained some attention, due to the difficulties involved with maintaining a strict minimum 12 hour fasting period. However, in case of an abnormal result, it is difficult to standardize the readings with the meal taken which is variable based on a person’s diet, and hence would invariably entail the patient to undergo the fasting test. Also, all the guidelines related to treatment of hyperlipidemia are standardized based on the results of a fasting lipid profile (3, 4).
Paras Pathology recommends its patients to have a strict minimum 12-hour fasting period to ensure the reproducible and comprehensible results.
How is my sample collected?
Sample collection for a lipid profile is in the usual manner, as for all blood tests. At Paras Pathology, sample for lipid profile is currently collected in a red capped tube, to which a label is attached bearing the patients details and a unique bar code.
What is tested?
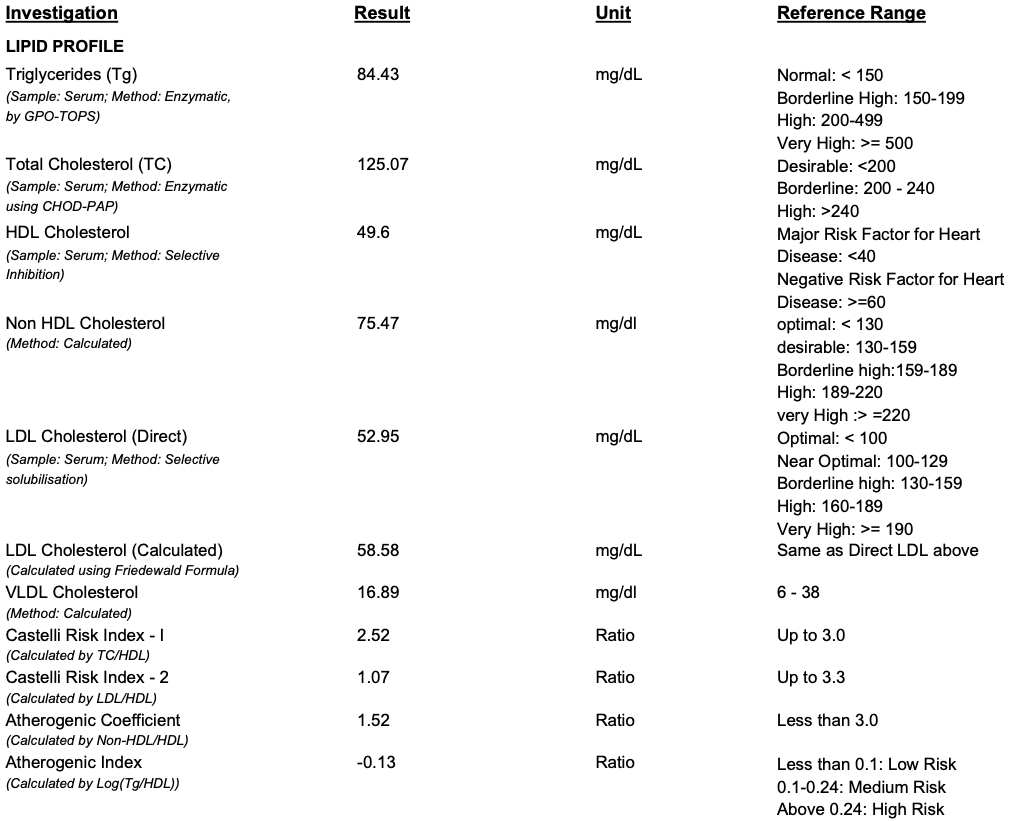
A lipid test is called a profile because of the variety of parameters covered as given below (picture shows an example of our new report format):
A. Triglycerides: After a meal, most of the fatty foods get converted to triglycerides, which are carried in the form of chylomicrons. In case of a heavy fatty last meal, or in case a patient doesn’t observe the recommended 12-hour fasting, this parameter is the most affected. As this parameter is directly affected by the immediately recent diet, this parameter may show the large variations in the same person in a matter of days. In the laboratory, this parameter is directly measured from the collected blood sample. High triglycerides is also target for cholesterol treatment, after LDL (3).
B. Total Cholesterol: This represents all forms of cholesterol present in your blood (different cholesterols described below, that is, HDL, LDL and VLDL). In theory, this value is the sum of all the different types of cholesterols. In the laboratory, this parameter is also directly measured.
C. HDL Cholesterol: This is commonly known as the “GOOD” cholesterol, as this is involved in “reverse cholesterol transport”, that is, it transports cholesterol from different parts of the body into the liver, for body function, thus helping in utilizing the cholesterol. As this REDUCES the cholesterol burden in the body, it is considered “good”, therefore, higher the HDL, lower the chances of health risk. This parameter too, is directly measured in almost all laboratories when you order a lipid profile.
D. LDL Cholesterol: This is commonly known as the “BAD” cholesterol, as this is type of cholesterol transports cholesterol from the liver to different parts of the body causing deposition of cholesterol at various unwanted places, like in our arteries, leading to the side effects of cholesterol, that is, clogging of the arteries (called “heart attack” when this happens in the heart, and “stroke” or “paralysis” when it happens in the brain).
This parameter is reported in two ways. Most laboratories report this parameter by calculation, using “Friedewald equation”, which gives a fairly good estimate, without having to directly measure this parameter. This helps in reducing the testing cost. However, as this equation uses triglycerides to estimate LDL, calculated LDL will also reflect the variations seen in triglycerides, which forms a disadvantage of using calculated LDL. Also, there studies also indicate that in many instances, the calculated LDL cholesterol may be over or underestimated as compared to the directly measured result (5, 6). There are multiple studies favoring direct measurement of LDL cholesterol, rather than from the formula, as LDL is the primary target of cholesterol lowering therapies (3). Hence, there are few laboratories that do measure this parameter directly, thus giving a precise value, rather than an estimate derived from a formula, but increases the cost of testing.
As LDL may be considered the single most important parameter in the lipid profile to be monitored, Paras Pathology has always reported directly measured LDL, and recently, we have started reporting both the directly measured as well as the calculated values (see attached picture)!
E. Non-HDL Cholesterol: Since most laboratories do not measure LDL directly, using non-HDL as a surrogate marker eliminates the variations of calculated LDL, as this parameter uses only total cholesterol and HDL cholesterol, both of which are relatively stable parameters over time. Thus, it is also considered a secondary target of therapy (3).
F. VLDL Cholesterol: This is the last type of clinically significant cholesterol that is reported. They are temporary molecules, formed during the process of lipid metabolism. VLDL result is always calculated from triglycerides.
G. Lipid Ratios: As our understanding of the lipid metabolism increased, scientists and doctors believed that, although the individual results are important, even when these are normal, some patients still ended up with some cardiovascular issues. This brought up the concept of “lipid ratios”, which are derived from more than one lipid parameter. The list of ratios are as given below:
a. Castelli Risk Index 1
b. Castelli Risk Index 2
c. Atherogenic coefficient
d. Atherogenic Index
Amongst the ratios mentioned above, the first two ratios, that is, the Castelli Index 1 & 2 are most commonly reported in almost all laboratories. In a given patient, a ratio can be abnormal, even though all cholesterol values are normal. Thus, the ratios are developed to help in better understanding the effects of all the different cholesterols, even when they are apparently normal. Hence, Paras Pathology reports all 4 types of ratios in its lipid profile report, as each have a significance, based on a particular patient profile.
Conclusion
Lipid profile forms one of the simplest, cost-effective, and one of the first line investigations in determining the cardiac risk of a patient. The entire test gives a lot of information, but that needs some basic understanding. Overall, the target is to reduce the “Bad” LDL cholesterol and keep the “Good” HDL cholesterol at a higher level. A directly measured LDL cholesterol should be preferred.
References
1. Wander, G.S., Jadhav, U.M., Chemburkar, A. et al. Lipid management in India: a nationwide, cross-sectional physician survey. Lipids Health Dis 16, 130 (2017).
2. Screening for Lipid Disorders in Adults: Recommendation Statement. Am Fam Physician. 2009 Dec 1;80(11):1273-1274.
3. Bethesda, et al. National Cholesterol Education Program. ATP III Guidelines at-a-Glance Quick Desk Reference, 2001.
4. Nigam PK. Serum Lipid Profile: Fasting or Non-fasting?. Indian J Clin Biochem. 2011;26(1):96-97.
5. Lindsey, C.C., Graham, M.R., Johnston, T.P., Kiroff, C.G. and Freshley, A. (2004), A Clinical Comparison of Calculated versus Direct Measurement of Low-Density Lipoprotein Cholesterol Level. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 24: 167-172.
6. Kannan S, Mahadevan S, Ramji B, Jayapaul M, Kumaravel V. LDL-cholesterol: Friedewald calculated versus direct measurement-study from a large Indian laboratory database. Indian J Endocrinol Metab. 2014;18(4):502-504.
Keywords : Cholesterol, Lipid Profile, Blood Tests, Pathology